OUR IMPACT
TYPE 1 DIABETES RESEARCH
David Breault, MD, PhD and Daniel Zeve, MD
David Breault, MD, PhD and Daniel Zeve, MD are working to unlock the potential of Gastrointestinal stem cells (GISC). Specifically, they are establishing a protocol to induce gastrointestinal stem cells into beta cells, evaluating the role of medicinal plant-derived factors to reprogram these cells, and develop a technique to yield insulin-producing cells from human gastrointestinal biopsies without direct DNA modification. Support of this project will help expand therapeutic treatment options for T1D patients.
In 2022 we are happy to announce we were able to donate $10,000 to support the work of Daniel Breault, MD PhD and Daniel Zeve, MD for research into Type 1 Diabetes at Boston Children’s Hospital.
CHILDHOOD CANCER RESEARCH
Grant Rowe, MD, PhD
Different types of leukemia show strong age biases. Leukemia affecting children is very different from that of adults. Grant Rowe, MD, PhD and his team are investigating these age differences, tying them back to the normal changes that occur in the blood forming system over time.
Dr. Rowe is interested in unlocking new paradigms of normal blood development with the long-term aim of building better models of childhood blood diseases. The process of blood formation changes over a lifetime: the blood stem cells formed in the embryo, newborn, child, and adult differ in their self-renewal and output of mature cells. He aims to understand the molecular regulation of how blood formation is ‘timed’ during development and aging and apply this knowledge to blood diseases, many of which are biased toward specific ages.
A recent blog article features Dr. Rowe’s work on B-cell ALL with rearrangements of the mixed lineage leukemia gene. He hopes to conduct similar studies for other forms of leukemia in the future.
Roberto Chiarle, MD
The innovative work of Roberto Chiarle, MD, could soon blunt the devastating toll of the deadliest form of childhood cancer, known as neuroblastoma. His strategy is to take each patient’s own immune system and teach it to go after a specific protein- ALK- that’s both unique to such cancer cells and required for their survival. In animal models, Chiarle has already shown that '“ALK-seeking” immune cells can target and kill the hardest-to-treat chemotherapy-resistant forms of neuroblastoma, a disease that accounts for 15% of cancer deaths in children worldwide. Now, the team is in the midst of switching from the discovery phase into clinical testing, an effort that could significantly boost chances of survival for millions of children around the world.
Our support will enable Dr. Chiarle to expedite the clinical trial. Because the ALK protein is expressed in the context of additional types of cancers, Chiarle’s work could have far reaching impact on a wide range of malignancies, including other solid tumors.
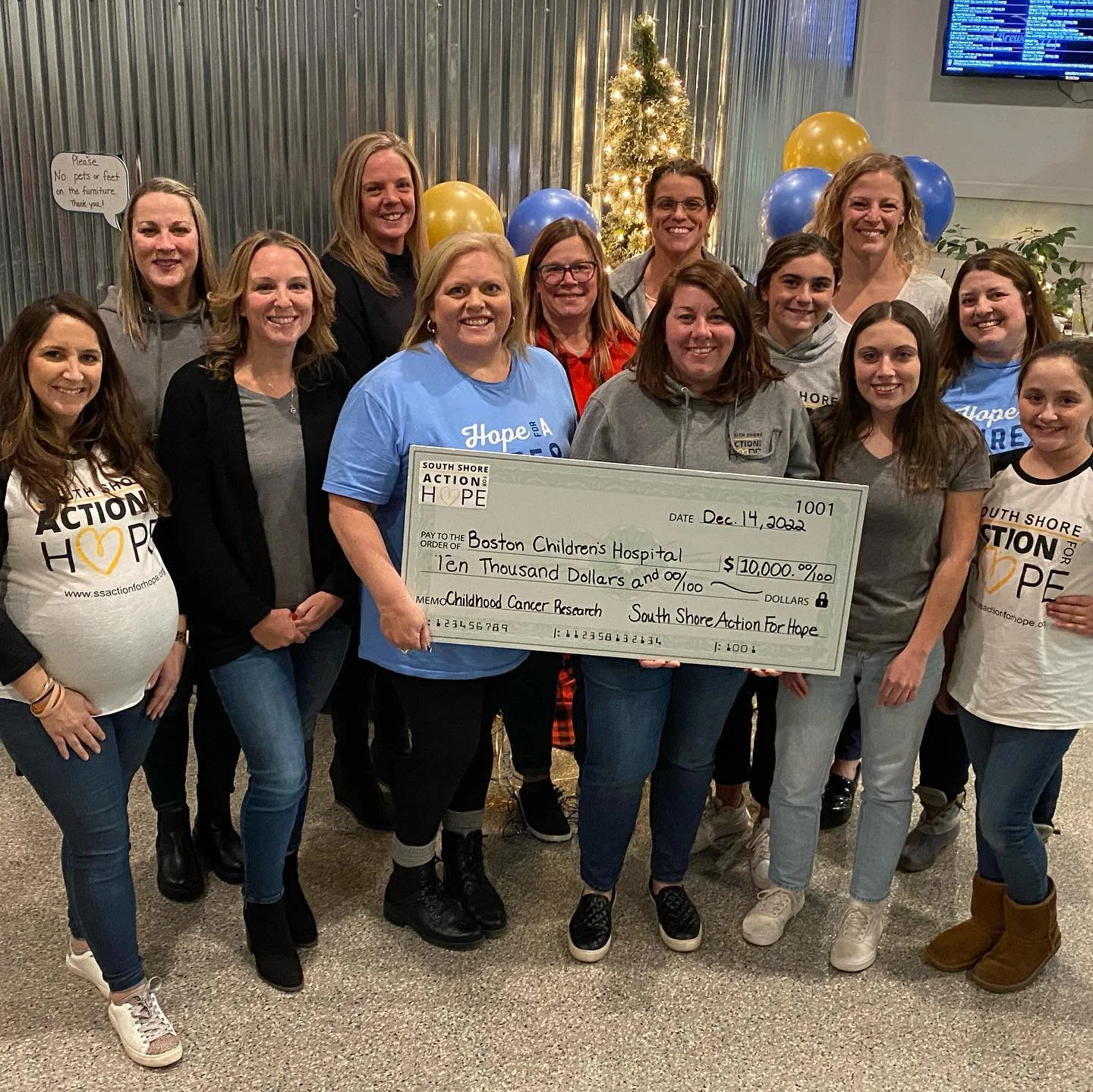
In 2022 we are happy to announce we were able to donate $30,000 to support the work of Roberto Chiarle, MD for childhood cancer research at Boston Children’s Hospital.
The generosity of our donors allowed us to support the following projects in 2021:
Boston Children’s Hospital
“Dr. Marsha Moses is tackling the most complex cancers in children and adults by creating personalized approaches through nanomedicine. One example involves Dr. Moses’ research in a challenging bone cancer called Osteosarcoma in children. Nanomedicine is the application of nanomaterials, or nanoparticles, to medicine. Nanoparticles are a form of transport for drugs and can go places drugs wouldn’t be able to go on their own. Nanoparticles can also be engineered and designed to package and transport drugs directly to where they’re most needed. This targeted approach means the drugs cause more harm in the particular, and intended, area of the tumor that they are delivered to. This minimizes collateral damage to surrounding healthy tissues and therefore the side effects.”
Joslin Diabetes Center
Lori Laffel, MD, MPH, Chief of the Pediatric, Adolescent and Young Adult Section at Joslin Diabetes Center, directs a range of studies, including a study showing the positive effect of continuous glucose monitoring for adolescent and young adult patients. Continuous glucose monitoring is tied to a smartphone app or display device and provides a reading every five minutes, with alarms to alert the user of high and low blood glucose levels or rapidly changing levels. For adolescents and young adults, who tend to have poor monitoring and control due to the life challenges associated with their age, continuous glucose monitoring has many long-term benefits. Studies such as this one are ensuring the best possible care and outcomes for pediatric and adolescent patients.
In addition, Dr. Laffel is overseeing an Artificial Pancreas Clinical Trial. This multi-center randomized clinical trial is evaluating a new artificial pancreas system — which automatically monitors and regulates blood glucose levels — and has found that the new system is more effective than existing treatments at controlling blood glucose levels in people with type 1 diabetes. The Joslin component of the study, led by Dr. Laffel, showed that the system improved participants’ blood glucose control throughout the day and overnight. The latter is a common but serious challenge for children and adults with type 1 diabetes, since blood glucose can drop to dangerously low levels when a person is asleep.